
EAPM News for Members April 2022
EAPM News is part of the EAPM membership and is as such exclusively sent to EAPM members about four times per year.
EAPM News April 2022
1 President’s address.
2 The Editor’s choice March 2022.
3 Prof James Levenson receives the Alison Creed Award 2022
4 Prof Wolfgang Söllner receives the Frits Huyse Award 2022
5 Meet our honorary members
5.1 Frits Huyse
5.2 Francis Creed
5.3 Ulrik Malt
5.4 Antonio Lobo
6 Join in! EAPM pages in the JPR
6 Join in! EAPM listserv
7 Calendar of events
1. President’s address

Jordi Blanch, EAPM President
Dear colleagues and friends.
I hope you are all well and with energy to continue with your hard work in these times.
It seems the COVID19 pandemic is decreasing, and this should allow all of us to return to the so-called “new normality”. However, Europe is still suffering from an old recurrent “illness”, which is a war and all its consequences on the general population. On our website you will find a short statement with our position and our concern on the mental health of many people and on the impact on the scientific cooperation
Nevertheless, the work and the activities of the EAPM continue as you will see in the present newsletter.
This year, Wolfgang Söllner has earned the Frits Huyse Award, whereas the Alison Creed Award goes to Jim Levenson. Natalie Uhlenbusch and Susanne Fischer, both young researchers and members of EAPM, conducted the interviews you can read in this newsletter.
We also introduce you, especially to the younger members among you, to our EAPM honorary members, namely Frits Huyse, Francis Creed, Ulrick Malt, and Antonio Lobo.
Last, few words to thank the enormous work of Chistoph Pieh and his team to make our next meeting in Vienna the best sign of the return to normality, but also the best example of networking, respect and collaboration between people of different countries.
Many thanks
Jordi Blanch i Andreu
President of the European Association of Psychosomatic Medicine
April 2022
2. The Editor’s choice March 2022
written by Jess G. Fiedorowicz, Editor-in-Chief, Journal of Psychosomatic Research, Professor and Senior Research Chair in Adult Psychiatry, University of Ottawa, Head and Chief of Mental Health, The Ottawa Hospital Scientist, Ottawa Hospital Research Institute, March 2022 and Antonina Mikocka-Walus, Deputy Editor, Journal of Psychosomatic Research .

Jess Fiedorowicz, JPR’s Editor-in-Chief
The Editor’s Choice –
“Identified Pathology Does not Impact Prognosis of Neurological Disorders”
This quarter’s Editor’s Choice article contrasts 12-month prognosis of patients referred to neurology clinics between those who had recognized pathophysiology or were deemed to have functional neurological disorders. There are several important clinical and advocacy take home messages from this article that warrant promotion with Editor’s Choice recognition. The selected paper analyzes baseline data from >2500 new neurology outpatients who participated in the Scottish Neurological Symptom Study (SNSS), a prospective, multi-centre cohort study in Scotland (1). From this sample 716 were classified as functional and 1865 as pathophysiological. The outcomes of each group at 12 months were nearly identical. Prediction models using deep neural networks training on 92 baseline features were not able to accurately predict outcome with an area under the receiver-operator curve of 0.67.
The medical community clearly treats those who present with symptoms with and without an explainable medical etiology quite differently. With regard to neurological symptoms, research has largely focused on nonepileptic seizures. Those without an identifiable medical etiology, sometimes called functional neurological symptoms, bear a considerable stigma (2) and even discrimination (3). Yet, these groups so segregated by the medical establishment have similar burdens from their illness (4). In this 12-month prospective cohort, they also have a strikingly similar prognosis. Based on change as measured by the Clinical Global Improvement scale, those with functional disorders were just as likely to experience improvement (32% vs. 34%), to remain unchanged (48% vs. 48%), or to worsen (19% vs. 18%). These are strikingly similar percentages which were not statistically significant (p=.52) even in this large sample.
The study sample is its clear strength: the cohort is representative of those receiving outpatient neurological care in Scotland across multiple centers. A total of 3,781 outpatients were recruited between 2002 and 2004. At baseline, the extent to which patients’ symptoms were attributable to an “organic” cause was assessed on a 4-point Likert scale. For the current analysis, these four categories were lumped into two: not at all/somewhat and largely/completely. For a clinical sample of this size, participants had a fairly comprehensive assessment at baseline, which included sociodemographic information, anxiety and depressive symptoms, health-related quality of life, sexual/menstrual symptoms, neurological symptoms, illness beliefs, illness experience, and causal attribution. The authors had at their disposal a large, reasonably well-characterized clinical sample in this prospective cohort.
Follow-up assessments were conducted at three and twelve months. The primary clinical outcome for this analysis was self-reported Clinical Global Improvement (much worse/worse/not changed/better/much better) at 12 months. As previously reported, the groups did not differ on this measure and were essentially indistinguishable. The authors also created models in attempt to predict outcomes from baseline variables using multiple methods, including deep neural networks. Models had quite limited predictive utility (AUC’s of 0.6-0.7) with older age, disease burden, and negative expectations as common predictors of outcome in both groups.
The work of Shipston-Sharmon and colleagues is a meaningful addition to a literature that should cause the broader medical community to rethink our approach to functional neurological disorders. These conditions can present across a full range of neurological symptoms but are more distressing and disabling than their medically explained counterparts. In a large, representative clinical sample, Shipston-Sharmon et al. show that while prognosis appears identical, and outcome is not easily predicted, the levels of anxiety and depression symptoms, quality of life and symptom burden are greater than in those with pathophysiological disorders. Functional neurological disorders can and should be treated with the appropriate resources, yet too often these patients are dismissed, even mistreated as they attempt to seek care for their condition. Often, they may not even have experienced a straightforward discussion of their diagnosis or prognosis. We must advocate, as others more eloquently have (5), for a healthcare system that provides these patients the interdisciplinary care and treatment they deserve, but too often remains reserved for those with identifiable etiologies and is out of reach.Seitenumbruch
References
- Shipston-Sharman O, Popkirov S, Hansen CH, Stone J, Carson A. Prognosis in functional and recognised pathophysiological neurological disorders – a shared basis. J Psychosom Res. 2021;152:110681.
- MacDuffie KE, Grubbs L, Best T, LaRoche S, Mildon B, Myers L, et al. Stigma and functional neurological disorder: a research agenda targeting the clinical encounter. CNS Spectr. 2020:1-6.
- Rawlings GH, Reuber M. Health care practitioners’ perceptions of psychogenic nonepileptic seizures: A systematic review of qualitative and quantitative studies. Epilepsia. 2018;59(6):1109-23.
- Carson A, Stone J, Hibberd C, Murray G, Duncan R, Coleman R, et al. Disability, distress and unemployment in neurology outpatients with symptoms ‘unexplained by organic disease’. J Neurol Neurosurg Psychiatry. 2011;82(7):810-3.
- Edwards MJ. Functional neurological disorder: an ethical turning point for neuroscience. Brain. 2019;142(7):1855-7.

Prof James Levenson receives the Alison Creed Award 2022
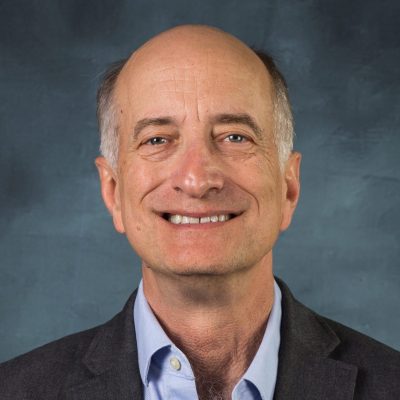
Prof James Levenson

Dr. Natalie Uhlenbusch
The interview was held on March 1st, 2022 between Prof James Levenson and Dr Natalie Uhlenbusch
Natalie Uhlenbusch: You won the Alison Creed Award for your outstanding life time achievements in the field of Psychosomatic Medicine / Consultation Liaison Psychiatry – Congratulations!
With over 200 papers and book chapters as well as seven books and several awards in teaching and research, you are a true luminary in the field of psychosomatic medicine/consultation liaison psychiatry. When and why did you decide that you wanted to dedicate your work to this subject?
James Levenson: Well, I already had some interests in psychology in college. I was very much a science student; I took a course in which in 10 weeks we read 3000 pages of Freud. So I entered medical school very interested in the interface between psychology and medicine. But I was uncertain if I wanted to be a pediatrician who knew a lot of psychiatry or a child psychiatrist who knew a lot about pediatrics, or an internist with a lot of knowledge in psychiatry or a psychiatrist with a lot of knowledge in internal medicine. And during my pediatric rotation I found routine pediatrics boring, and many of the interesting cases too upsetting, so I decided that it’s got to be somewhere between internal medicine and psychiatry. Then I started out in an internal medicine residency and after a year switched into psychiatry. I realized that consultation liaison psychiatry and psychosomatics was a way of having a foot in both worlds. I also knew a personal trait of mine, and there’s a positive and a negative way to look at this trait, like most human traits. The positive perspective is that I have very diverse interests. The negative perspective is that I get bored doing just one thing. Consultation liaison psychiatry was also a way then to align my career with my personality.
Are there any moments in your career so far that have been particularly memorable for you?
That’s a hard question because there have been so many! It was very gratifying to lead the way in getting consultation liaison psychiatry recognized as an official subspecialty of psychiatry in the U.S. It was a tremendous honor to be chosen as an editor of Journal of Psychosomatic Research. There are many other memorable moments, such as the publication of the first edition of my Textbook on Psychosomatic Medicine, that certainly was very gratifying.
A personal memory, which is in some ways is a small thing but at the same time it is not a small thing, was the very first time I came to the EAPM. It was actually still a predecessor organization then and the meeting was in Berlin and Wolfgang Söllner was the host. And I was nervous about coming to Germany because I am Jewish and my parents wanted nothing to do with anything German – I am sure you can understand. But there at that meeting, Wolfgang had arranged a special session on psychiatrists’ complicity with the Nazis and I felt very much welcomed and at home. And this was the start of a friendship with Wolfgang and a number of other European psychiatrists which has been very important for me.
Thinking back to the moment when you graduated from medical school at the University of Michigan, has your professional journey turned out the way you had imagined it?
You know, I think it has, although I have never been one to have a 5-year plan, I just let things evolve kind of organically. And in that way I was influenced by my father who was a famous nuclear engineer. He had this amazing career and I asked him how it had happened and he said he never planned anything, he just tried to do good work and opportunities came his way. And that is how my career has unfolded, too. I just tried to do what was interesting and tried to do a good job and opportunities came my way, but I never really had an exact vision.
Is there anything that you would recommend to young scientists in the field?
Well, I think that there was a time in academic medicine when one could try to do everything, be a clinician, be a teacher, be a researcher. In fact, at least in the US back then, being an expert in all those things was called being a triple threat, which is actually a sports metaphor. But it’s really not possible to have equal excellence in all those things and so you have to make some choices and decide what it is that gives you the greatest pleasure. I actually have not fulfilled my research potential because I have devoted so much time to clinical work and teaching. And I am happy with that but it did require some decisions along the way, which were the right decisions for me but would not have been the right ones for everyone.
And what did you base these decisions on?
If I’m being honest, it was a mixture of not wanting to be too narrowly focused, not wanting to give up or greatly reduce my clinical work and teaching but also some anxiety about putting all my eggs in one basket. It made me too nervous to put all my eggs in the basket of applying for grants. Anxiety played a role in staying involved in research but also staying very committed clinically and in teaching.
Are there any exciting current projects that you would like to tell us about?
I am excited that at my age I am still well enough to be just as busy as I’ve ever been, teaching, seeing patients. Most of my colleagues don’t know that in addition to the other things I do, I have chaired our health systems’ ethics committee for 33 years and I provide most of the ethics consultations in the hospital. And I am excited to be able to continue to assist my colleagues with difficult cases whether complex psychiatric cases or in ethical dilemmas. So yeah, I am just happy that I can continue doing all the things I did before.
One of your research interests are psychiatric disorders in the medically ill. Based on your clinical and research experience, what is essential in maintaining mental health despite a physical condition? What can and should we as healthcare professionals do to support patients in the best possible way?
That’s a book!
Well, I think one of the things that is relevant on an organizational level – I don’t know much about medical education in other countries – but if I were in charge of the education of medical students and residents, I think programs should reflect the proportion of psychopathology, psychiatric problems and psychological distress that they will encounter in their patients. And it’s far from that. One can go through internal medical training in the United States and learn nothing about psychiatry. And yet, depression is the most common diagnosis they will end up treating in primary care. I think one of the things we have to do is try to break down the barriers between the disciplines. Too many psychiatrists come out of their training not feeling very comfortable with their medical knowledge. But non-psychiatrists – at least in the US – their level of knowledge about the most common things, such as delirium, dementia, schizophrenia depression etc., is terribly limited and that’s a major educational failure.
We live in turbulent and somewhat disturbing times we live in. The war in Ukraine, the COVID-19 pandemic, the climate crisis, all these are threats that can have a significant impact on physical and mental health. What role do such political events play in the context of your work?
Until Donald Trump was elected president in the US, I was very careful to be politically neutral with my patients and to never discuss politics with them. They were not there to discuss politics but to receive care. I also didn’t want my politics to be visible to patients because I wanted to be able to take care of every kind of patient regardless of their political or religious views. But during Trump’s presidency, there was widespread endorsement by him and other leaders of racism, sexism, xenophobia, homophobia… and I decided that I could not be silent in the face of those things when they would come up with a patient. And that’s because those aren’t political issues alone; those are social diseases. And I remember all the way back in medical school, reading about Virchow, who was the founder of modern pathology, and he also was in many ways the founder of public health medicine, and he said that it was a physician’s responsibility to address the social causes of diseases. By the way, he lost his university position because he was a communist and used his position very publicly to advocate for better working and living conditions for poor people. So I think things like what’s going on in Ukraine force all of us to confront these questions. There are some things to be silent in the face of means to tacitly endorse them.
Prof James Levenson receives the Alison Creed Award 2022. Meet him in the interview.
Find out more about Prof Jim Levenson
At the EAPM 2022 Vienna Conference, Prof James Levenson will give a plenary lecture on “A History of Consultation-Liaison Psychiatry in America: A Personal Perspective. He will also give a masterclass on “Psychopharmacology in the Medically Ill”.
4. Prof Wolfgang Söllner receives the Frits Huyse Award 2022

Prof Wolfgang Söllner

Dr Susanne Fischer
The interview with Prof. Wolfgang Söllner was conducted by Dr. Susanne Fischer held on March 8th, 2022.
Dr Susanne Fischer: Dear Professor Söllner, my heartfelt congratulations to you for winning the Frits-Huyse-Award. What does it mean to you to be awarded this prize?
Prof Wolfgang Söllner: I feel deeply honoured to be the recipient of this award. To me, it represents a recognition of my efforts to bring together European researchers and clinicians in psychosomatic medicine and consultation-liaison psychiatry. The fact that this is a European prize is particularly important to me as we are currently witnessing times in which the very existence of Europe is threatened by the current political developments. The award also means a lot to me because of my long-standing friendship and collaboration with Frits Huyse, whom I have always admired for his tenacity in pursuing the research topics that mattered the most to him.
May I ask what initially drew you to the field of psychosomatic medicine and consultation-liaison psychiatry? And what has kept you fascinated until this day?
When I was just 17 or 18 years old and in school, I was already fascinated by psychoanalysis. However, I realised that I was also intrigued by the natural sciences and thus started to study medicine at the University of Innsbruck, Austria. After my studies, I begun to train in family medicine. During this time, in which I rotated between different medical departments, I realised that it was the personal stories of the patients which they told me during my visits that resonated with me the most. When did someone fall ill? Why did they develop that particular illness? What could the patient learn from their illness? These were the questions I asked myself. Given this increasing interest in the associations between psychosocial factors and somatic diseases, I decided that I wanted to become an internist with a focus on psychosomatic medicine. After a research and clinical year at the University of Heidelberg, a forerunner in psychosomatic medicine in Germany, I moved back to Innsbruck for personal reasons. It was there where I had the unique opportunity to build an psychosomatic outpatient clinic with Wolfgang Wesiack, a famous internist, psychoanalyst, and Professor of Psychological Medicine at the University of Innsbruck. Together with a colleague, I was also able to develop a consultation-liaison service at the University Hospital in Innsbruck. We started with patients with chronic pain and then moved on to oncological patients. The collaboration with colleagues from medical and surgical departments, for example during consultation hours, in research projects and in the teaching of medical students, has been one of the most rewarding experiences in my career. To this day I feel that there is hardly anything more exciting than to work at the intersection between somatic and psychological medicine. No two patients are alike and there is something to learn from each case.
Among your many seminal contributions to psychosomatic medicine and consultation-liaison psychiatry, for example, in your role as President of the EAPM, which ones do you personally regard as most important?
I feel that contributing to international networks in the field has been among my most formative experiences. One important network which I helped to create was the European Consultation-Liaison Workgroup, which conducted research into patient-centred care across 14 different countries in Europe. The purpose of this programme was to identify the ingredients of successful approaches of integrative care. The second network I contributed to was the INTERMED work group. This was an attempt of creating ways towards a structured assessment of biopsychosocial aspects of each individual patient. As part of this group, I participated in developing instruments for the bio-psycho-social assessment of patients with complex diseases and helped to evaluate them in different patient populations. These experiences also brought me to EAPM in the end, which originated from these study groups, and brought together psychosomatic medicine and consultation-liaison psychiatry. As a representative of both fields, I could contribute to joining these two traditions and to become the society’s first president. From a research point of view, working with patients suffering from severe somatic diseases and who were under existential threat has always felt particularly meaningful to me and I have recently edited a book on psychotherapy with the medically ill that is devoted to this topic.
You have obviously been extremely successful in building a meaningful career in psychosomatic medicine and consultation-liaison psychiatry. Could you name the main “ingredients” of this success?
Clinically, I believe that it was important to build interdisciplinary structures, as we have done in Innsbruck and continued to do at the Paracelsus Medical University in Nuremberg, Germany. Building bridges, identifying common interests with our clinical colleagues, and conceiving of ways how consultation-liaison psychiatry can be most useful for the day-to-day work of these people has been key to ultimately deliver high-quality clinical care. You also need stamina and a vision to guide your work. The same applies to research. Networking and communication are a sine qua non and you need motivated people from different professions, each contributing their specific expertise. Personally, it has also been important to me to have role models, such as Wolfgang Wesiack, my first mentor. He was the one who taught me that there is something to learn from each patient. Frits Huyse, Fritz Stiefel, Francis Creed, and Jim Levenson have greatly impressed and inspired me for many years. If I had to give any advice to early career researchers in psychosomatic medicine and consultation-liaison psychiatry, I would say that it is important to walk on both legs, basic research and clinical practice. Basic researchers need to be thinking about the clinical relevance of their work and clinical practitioners should have a sound methodological knowledge to evaluate their models of integrated care.
Which projects are you currently working on? And: Are there any specific areas in psychosomatic medicine and in consultation-liaison psychiatry where you would like to see more progress in the near future?
A meta-analysis of our group published in Psychotherapy and Psychosomatics has shown that consultation-liaison services are effective in alleviating depression and anxiety in the medically ill. However, what we still know little about is to what extent our liaison work helps to improve hospital teams. One project I am currently involved in addresses this important gap in the literature. In future studies, I would also like to see more research in Europe into the efficacy of collaborative care, which connects inpatient and outpatient treatment. A second project I am excited about is my work on philosophical and ethical aspects of psychotherapy in the medically ill, parts of which I have summarised in my latest book. I believe our profession will be key to tackle at least three major healthcare-related challenges. First, the prevalence of mental disorders will further increase and new psycho-somatic or somato-psychic disorders, such as Long-Covid, will emerge, which will require our expertise. Second, digitalisation and artificial intelligence will have a massive impact on medicine, and in particular on the doctor-patient relationship. I am convinced that we will have a key role in improving communication both between patients and doctors as well as within teams. Finally, the borders between disciplines will continue to dissolve and our profession is uniquely positioned to help to overcome this structural challenge due to our long-standing experience of working at the interface between the body and the mind.
Prof Wolfgang Söllner receives the Frits Huyse Award 2022. Meet him in the interview.
Find out more about Prof Wolfgang Söllner
At the EAPM 2022 Vienna Conference, Prof Wolfgang Söllner will give a plenary lecture.
5 . Meet our EAPM Honorary Members
5.1 Prof Frits Huyse
Prof. Frits Huyse
‘In 1983 when I registered as a psychiatrist in The Netherlands C-L psychiatry as an organized form of psychiatric service delivery in the general hospital in Europe was sparsely available. No national organization’s, no international meetings, no guidelines. However there were individual psychiatrist who were very dedicated to the psychiatric care of the medically ill.
By obtaining a EU-grant to do a service delivery study Ulrik Malt, Antonio Lobo, Thomas Herzog and I were able to create a European C-L network covering 11 countries and 56 C-L services which provided both psychiatric- and psychosomatic care for the medically ill.
Later joined by Peter de Jonge, Fritz Stiefel, Wolfgang Söllner, Silvia Ferrari, Beate Wild, Elena Lobo, Joris Slaets, Annet Boenink, Corine Latour and Roger Kathol (ACLP) our group was able to develop an integrated risk assessment- and management system called the INTERMED.
In the course of the years these initiatives appeared to be part of a globalized effort to improve the quality and extent of C-L research and service delivery, specifically the international collaboration which is so characteristic for the meetings of the EAPM, nowadays attended amongst other by our American-, Australian- and Japanese colleagues.’ (Frits Huyse, 2022)
5.2 Prof Francis Creed

Prof. Francis Creed
As a Professor of Psychological Medicine at University of Manchester, UK, I helped develop C-L Psychiatry nationally and developed a portfolio of research concerning mind-body relationships upon which we based clinical trials to improve psychological treatment for patients in the General Hospital.
My work was multidisciplinary: Else Guthrie, Chris Dickens, Barbara Tomenson and Wendy Clarke were my closest colleagues, but I worked with many physicians, other health scientists and PhD students, 10 of whom are now professors! I was Editor of the Journal of Psychosomatic Research for 12 years and I treasure the collaborations and friendships I developed in my time as President and Treasurer of European Association of Consultation-Liaison Psychiatry & Psychosomatics, now EAPM.
4.4 Prof. Ulrik Malt

Prof. Ulrik Malt
Malt received his medical education at the University of Münster (Germany) and University of Oslo (Norway) and specialized in psychiatry. He has been professor of psychiatry, medical faculty, University of Oslo since 1988 and was head of Department of Psychosomatic medicine and C-L psychiatry, Oslo University Hospital (Rikshospitalet) from 1988-2014.
Together with Frits Huyse (Amsterdam), Antonio Lobo (Zaragoza) and Thomas Herzog (Freiburg), Malt was actively involved in obtaining EU-funding for C-L psychiatry in Europe [European Community 4th Medical and Health Research Program COMAC-Health service research]. He was also involved in further organizational development of C-L psychiatry and psychosomatic medicine in Europe (European Association for Consultation Liaison Psychiatry and Psychosomatics – EACLPP; European Association of Psychosomatic Medicine – EAPM).
For many years Malt was the European representative on the program committee of the annual meetings of the US-based Academy of Psychosomatic Medicine (current name Academy of Consultation-Psychiatry). Malt founded EAPM’s Frits Huyse Award for outstanding lifetime achievements promoting and strengthening European C-L psychiatry and psychosomatic medicine research.
4.5 Prof. Antonio Lobo

Prof. Antonio Lobo
Chair of Psychiatry, now Emeritus Professor, University of Zaragoza, Spain.
Formerly Chief of the Psychiatric Service, Hospital Clínico Universitario, Zaragoza
- Graduate (1971) and Doctorate (1972), University of Zaragoza.
- Grants: CSIC (Superior Council of Scientific Research, Ministry of Universities); British Council, Maudsley Hospital and Psychiatry Institute, University of London.
- Residency training, New York Hospital-Cornell University Medical School. (1973-76)
- Attending Psychiatrist and Instructor, Johns Hopkins Hospital and Medical School, EE.UU.(1977)
- Founded in 1977 the first Psychosomatic and Liaison Psychiatry Unit in Spain, in the University Hospital
- Visiting Professor: Johns Hopkins University; Iowa University, USA
- Research areas with “impact” and systematic publications in Psychosomatic and Liaison Psychiatry, and in Dementia-Psychogeriatrics.
- Principal Investigator in Spain: European Union Projects European Consultation-.Liaison Workgroup (principal investigator Frits Huyse)
- National Coordinator of the Research Thematic Network in Psychosomatic and Liaison Psychiatry (National Research Institute, Instituto de Salud Carlos-III)
- Member of the Scientific Council (ISC-III) and the National Committee of the Specialty of Psychiatry (Ministry of Health)
- Former President, Spanish Society of Psychosomatic Medicine.
- First president of the European Association for Consultation-Liaison Psychiatry and Psychosomatics
- Editor-in-Chief, The European Journal of Psychiatry. Member of the Editorial Board: Journal of Psychosomatic Research, International Journal of Psychogeriatrics, International Review of Psychiatry, others
Awards (Professional career):
Sociedad Española de Psiquiatría Geriátrica, SEPG (2013); Sociedad Española de Medicina Psicosomática , SEMP (2013), Ilustre Colegio Oficial de Médicos de Zaragoza. (2017); First “Frits Huyse Award”, European Association for Psychosomatic Medicine, EAPM (2014)
6. Join in! : EAPM pages in the Journal of Psychosomatic Research
A section of the journal is devoted to topics of particular relevance to EAPM.
As part of the agreement with the Journal of Psychosomatic Research, EAPM has a quota of 48 pages per year for EAPM-related matters, including papers, letters, news, advertisements, publications of C-L activities in various European countries and much more.
EAPM members are invited to submit papers for the EAPM pages to ensure that we make full use of our pages. Instructions for authors can be found below.
Click → here for the EAPM pages.
Instructions for authors of EAPM pages
EAPM contributions should not exceed 1000 words. Contributions are not meant to publish results of specific disease-related research; topics covered should be of general interest, stem from countries participating in the EAPM or refer to EAPM activities. EAPM contributions are not peer-reviewed but subject to editorial approval. In case of doubt about the suitability of a subject, please contact Prof. Else Guthrie (eapm-pages@eapm.eu.com), Associate Editor for EAPM pages.
Submit your article for EAPM pages NOWYou will be redirected to the JPR's Editoral manager
8. Join in! – use our listserv
The EAPM members’ clinical network list is intended for all individual EAPM
members to exchange information among themselves. Each EAPM member can use this
list to get advice on clinical issues, but also to collaborate or exchange on
research. References to relevant studies, as well as expressions of interest, words of encouragement, or questions can be exchanged. The list is maintained by the EAPM.
Send a message to EAPM members via our listserv, mail to: EAPMMEMBERSCLINICALNET@HOME.EASE.LSOFT.COM
4.8 Calendar of Events
Do you have a date for us that you would like to add or share? For example, a meeting in your country? Please do not hesitate and send it to our administration:contact@eapm.eu.com
EAPM Conference Vienna 2022
9th Annual Meeting of the EAPM
8-11 June 2022
Language: English
Royal College of Psychiatrists: International Congress 2022
International Congress 2022
20-23 June 2022
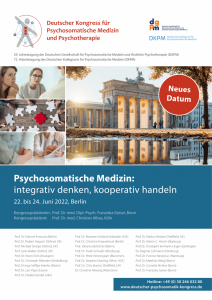
German Congress of Psychosomatic Medicine (DKPM/DGPM)
Annual Meeting
22-24 June 2022
Language: German/English
EAPM lectures
September 2022
ICPM 2022
World Congress of the International College of Psychosomatic Medicine
Language: English
Rochester, NY, USA
October 2022
Network Eating Disorders / Austria International Congress 2022
Network Eating Disorders / Austria
29th Annual Conference
Language: German/English
November 2022
ACLP 2022 Conference
CLP 2022 Conference
Annual Meeting of the Academy of Consultation-Liaison Psychiatry (ACLP)
November 10 – November 12, 2022
CLP 2022
June 2023
EAPM Conference Wroclaw 2023
10th Annual Meeting of the EAPM
14. – 17. June 2023
Language: English






0 Comments